
April 19, 2024
Cholestatic Liver Disease: Symptoms, Diagnosis, and Treatment
Cholestatic liver diseases (CLDs) are a group of conditions characterized by jaundice and cholestasis, which can lead to complications like end-stage liver disease and cirrhosis. Cholestasis occurs when bile formation, secretion, or excretion is impeded due to intrahepatic or extrahepatic factors.
The Saudi Association for the Study of Liver Diseases and Transplantation has created guidelines to provide standardized care for patients with cholestatic liver disease. This article will discuss the symptoms and diagnosis of cholestatic liver disease, as well as the available treatment and management options.
Understanding Cholestatic Liver Disease
Intrahepatic Cholestasis
Caused by chronic liver diseases, acute hepatitis, pregnancy, total parenteral nutrition, or certain medications. Characterized by dysfunction of hepatocytes, bile canaliculi, canals of Hering, bile ductules, or cholangiocytes, without obvious bile duct obstruction.
Extrahepatic Cholestasis
Caused by biliary strictures or bile duct obstructions. Characterized by obstruction or injury to the septal, regional, segmental, or common bile ducts
Types and Causes of Cholestatic Liver Diseases
| Acute Causes | Chronic Causes |
| Common bile duct stones | Primary sclerosing cholangitis |
| Cholangitis | Primary biliary cholangitis |
| Drug-induced liver injury | Secondary sclerosing cholangitis |
| Sepsis | Biliary atresia |
| Intrahepatic cholestasis of pregnancy | Rare infiltrative disorders |
| Total parenteral nutrition-associated cholestasis | Paraneoplastic syndromes |
Hereditary cholestatic liver diseases, such as cystic fibrosis-associated liver disease (CFLD), familial intrahepatic cholestasis (FIC), and Alagille syndrome, are also known to occur.
Primary Biliary Cholangitis (PBC) and Primary Sclerosing Cholangitis (PSC)
- PBC is a chronic, autoimmune disease characterized by cholestatic elevation of liver enzymes and positive antimitochondrial antibody (AMA).
- PSC is a chronic, idiopathic, cholestatic disease that often progresses to end-stage liver disease.
- Both PBC and PSC are slow progressive chronic cholestatic liver diseases caused by bile duct destruction and fibrosis leading to cirrhosis.
Symptoms and Diagnosis
Symptoms of Cholestatic Liver Disease
The primary symptoms of cholestatic liver disease are indicative of the buildup of bile and bilirubin in the body due to impaired bile flow:
- Jaundice (yellowing of the skin and whites of the eyes) due to elevated bilirubin levels in the blood.
- Light-colored, fatty stools (steatorrhea) due to lack of bile in the intestines for fat digestion.
- Pruritus (severe itching) caused by the accumulation of bile salts in the blood
- Dark urine.
- Other symptoms may include abdominal pain, nausea, vomiting, and fatigue.
Diagnostic Evaluation
The diagnosis of cholestatic liver disease involves a combination of blood tests, imaging studies, and sometimes invasive procedures:
Blood Tests:
- Elevated levels of bilirubin, bile salts, cholesterol, and liver enzymes like gamma-glutamyl transferase (GGT) and alkaline phosphatase (ALP).
- Diagnosis of cholestasis is made when ALP exceeds 1.5x the upper limit of normal (ULN) and GGT exceeds 3x ULN.
Imagine Test:
- Abdominal ultrasound, CT scan, or HIDA scan to visualize the biliary system and detect obstructions or inflammation.
- Magnetic resonance cholangiopancreatography (MRCP) is the preferred imaging technique for Primary Sclerosing Cholangitis (PSC) diagnosis.
Exploratory Procedures:
- Endoscopic retrograde cholangiopancreatography (ERCP) or endoscopic ultrasound (EUS) to directly examine the bile ducts if routine imaging is inconclusive.
- Liver biopsy to analyze a sample of liver tissue and diagnose conditions like small duct PSC or exclude other causes.
Diagnosis of Specific Cholestatic Liver Diseases
- Primary Biliary Cholangitis (PBC): Elevated ALP combined with positive antimitochondrial antibody (AMA) titer >1:40, or specific antinuclear antibodies (ANA) in AMA-negative patients.
- Primary Sclerosing Cholangitis (PSC): MRCP is the preferred diagnostic technique, and liver biopsy may be used to diagnose small duct PSC or exclude other conditions. Patients with PSC and inflammatory bowel disease (IBD) should undergo regular surveillance colonoscopy to screen for colorectal neoplasia.
Treatment and Management
Treatment Principles and Medications
The main treatment principles for cholestatic liver disease are addressing the underlying etiology and managing symptoms. Several therapeutic drugs are used in the management of cholestatic liver diseases:
Ursodeoxycholic acid (UDCA):
- First-line treatment for primary biliary cholangitis (PBC) at 13-15 mg/kg/day.
- May delay disease progression in PBC, but liver transplantation is potentially curative.
- Not recommended for primary sclerosing cholangitis (PSC) as it has not shown clear benefits.
Obeticholic acid (OCA):
- Second-line therapy for PBC patients with inadequate response to UDCA.
- S-adenosyl-L-methionine (SAMe), cholestyramine, and fibrates: Used as adjunctive therapies in cholestatic liver diseases.
Glucocorticoids and immunosuppressants: May be considered for refractory cases.
Management Strategies
- Risk Stratification: Important for identifying high-risk PBC patients with suboptimal UDCA response, who may require second-line therapy like OCA or bezafibrate.
- Dietary Modifications: Dietary substitution is the main treatment for fat malabsorption, including a diet rich in carbohydrates and proteins or medium-chain triglycerides in infants. Lifestyle changes like diet, exercise, and avoiding alcohol can help slow disease progression in chronic cholestasis.
- Vitamin Supplementation: Careful monitoring and supplementation of fat-soluble vitamins (A, D, E, K) is crucial in chronic cholestasis to prevent deficiencies.
- Endoscopic and Surgical Interventions: Endoscopic treatment with balloon dilation is recommended for dominant strictures in PSC. Surgery may be an option to remove or replace severely damaged organs in some cases.
- Liver Transplantation: Considered for PBC patients with MELD score >12 or total bilirubin >103 μmol/L. Considered for PSC patients with decompensated cirrhosis or severe recurrent bacterial cholangitis.
- Monitoring and Referral: Close monitoring for cholangiocarcinoma and colorectal cancer is essential in PSC patients. Referral to a gastroenterologist or hepatologist is indicated for severe or prolonged cholestatic liver disease.
Conclusion
Cholestatic liver diseases encompass a range of conditions that impair bile flow, leading to the accumulation of bile and bilirubin in the body. Early recognition of symptoms like jaundice, pruritus, and steatorrhea, along with diagnostic tests like liver enzyme analysis and imaging studies, is crucial for accurate diagnosis and timely intervention.
The management of cholestatic liver diseases involves addressing the underlying etiology, controlling symptoms, and preventing complications. Pharmacological therapies like ursodeoxycholic acid and obeticholic acid play a vital role, alongside dietary modifications, vitamin supplementation, and endoscopic or surgical interventions in specific cases. Liver transplantation remains a potentially curative option for advanced or refractory cases. Ongoing monitoring for disease progression, complications, and associated malignancies is imperative for optimal patient outcomes.
FAQs
1. What are the treatment options for cholestatic liver disease?
To manage cholestatic liver disease, dietary modifications and supplements can be important to offset malabsorption issues and vitamin deficiencies. Additionally, Ursodeoxycholic acid, a medication primarily used to dissolve gallstones, may be prescribed. This drug can aid in increasing bile production and alleviating the impact of excess bile salts in the bloodstream.
2. How is cholestatic liver disease identified and diagnosed?
Diagnosing cholestatic liver disease involves a comprehensive medical history and physical examination. Noninvasive radiological tests such as ultrasound, computerized tomography (CT) scans, and magnetic resonance cholangiography are instrumental in diagnosing, especially when the disease originates outside the liver (extrahepatic).
3. What signs indicate the onset of liver disease?
Early warnings of liver disease can include jaundice, which is the yellowing of the skin and the whites of the eyes. This symptom might be less noticeable on darker skin tones. Other signs include abdominal pain and swelling.
4. What are the consequences of untreated cholestasis?
Neglecting to treat cholestasis can lead to severe complications such as fibrosis and biliary cirrhosis, progressing eventually to end-stage liver disease.

Written By
Shafiq Ahmad Khan
Founder & CEO
Recents Posts
-

7, May 2024
Kshar Sutra Therapy: Ancient Ayurvedic Remedy for Piles and Fistula Healing
-

30, April 2024
Ayurveda Treatment in India
-

26, April 2024
Best Liver Transplant Surgeons in India
-
24, April 2024
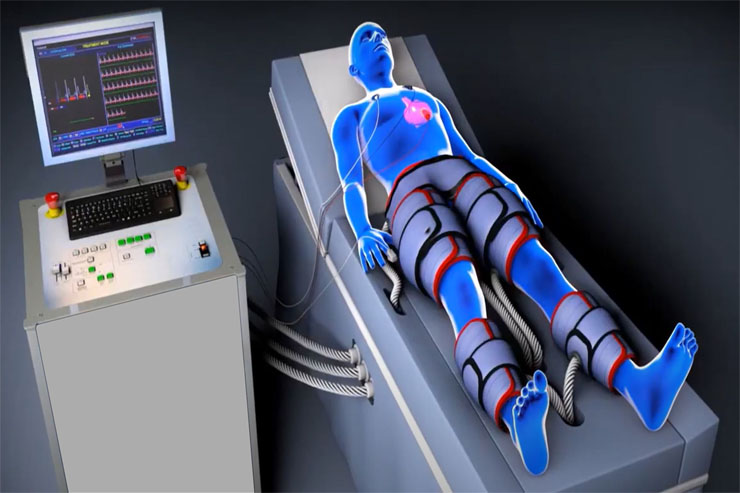
Power of EECP Therapy: A Revolutionary Approach to Heart Health in India
-

19, April 2024
Cholestatic Liver Disease: Symptoms, Diagnosis, and Treatment


